EYE HEALTH
WE’RE GETTING PERSONAL
Here at Hansen Optometrists we believe in equal eye care for everyone, treating each patient’s eyes with personal care.
We have everything you need to ensure you and your family have good vision for life, using the latest in examination technology.
With our highly trained team of experts, we will give you what your visual needs require.
At Hansen Optometrists we use the latest in examination technology. We want to make sure our patients have the best vision care possible and with that we are proud to say we are one of the most clinically and technologically advanced practices in Australia.
We provide the following examination technologies;
- Digital Retinal Scan
- Visual Field Testing
- Ocular Coherence Tomography (Oct)
- Laser Auto Refraction
- Corneal Topography
- Colourimetry
COMMON EYE CONDITIONS
Here we have a look at the most common eye conditions that can affect anyone, at any age, though they are more likely to occur as we get older. We have included a short definition of the condition but with a short click we can have a more in depth look.
- Digital Eye Strain – is the physical discomfort of the eye that is felt after excessive exposure to digital devices, including; smartphones, laptops, tablets, etc.
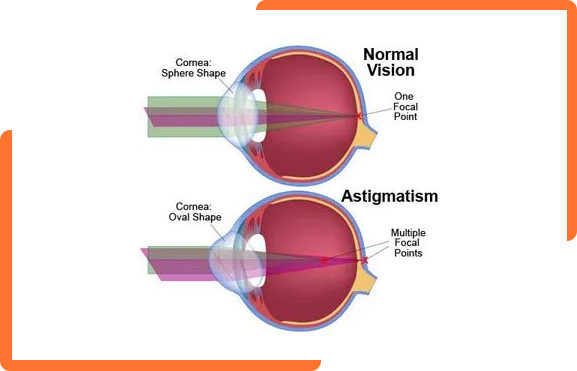
- Astigmatism – is when the cornea is more almond shaped rather than spherical, this causes distorted images.
- Presbyopia – is when the lens of the eye loses its elasticity causing long-sightedness, this typically occurs in middle-aged patients.
- Myopia (near/short-sightedness) – is when the light that comes in does not focus on the retina but in front of it, causing distance vision to be out of focus.
- Dry Eye – is when there is an inflammation of the cornea of the eye and conjunctiva, this is due to inadequate tear secretion.
- Glaucoma – is when there is increased pressure within the eye, which then causes gradual loss of sight.
- Cataracts – is when the lens of the eye starts to cloud due to the tissue breaking down and proteins in the eye starting to clump.
- Macular Degeneration – is a group of degenerative diseases of the retina, which cause progressive and painless loss of central vision.
- Ocular Therapeutics – is the diagnosis and treatment of ocular conditions.
DIGITAL EYE STRAIN
Digital eye strain is the physical discomfort felt after prolonged time in front of digital screens.
Did you know the average adult;
- Looks at least 3 different digital screens every day.
- Looks at their smartphone or iPad up to 60 times per day.
- Spends at least 12 hours a day consuming some form of media form a digital screen.
So it is no surprise that staring at screens throughout the day can be hard on your eyes and may cause digital eye strain — even if you don’t currently wear glasses. Because screens are small, bright and we spend a lot of time staring at them, they make our eyes work hard.
Here are some of the most common conditions you can experience by staring at screens for too long:
- Dry Eyes - when you look at something up close (eg your smartphone)you reduce your blink rate, which can cause dry irritated eyes.
- Eye Strain - also known as ‘eye fatigue’ – can cause headaches, red, irritated eyes and neck or back pain.
- Headaches - usually frontal (across the top of head) or to the temples (side of head) after prolonged close work.
How to protect yourself
- Good Visual Hygiene - Take frequent breaks; watch your working distance and good lighting.
- Protect your eyes against harmful blue light radiation from digital screens.
- Use specialised lenses called Anti-Fatigue for all device use.
WHAT IS MYOPIA?
Myopia (short-sightedness) is one of the most investigated areas within vision science. Yet we still do not fully understand why myopia develops and how to stop it.
POSSIBLE CAUSES
- For myopia to occur the eyeball has to grow longer (change in axial length).
- In the past this axial length change was considered to be due to genetics, as myopia tends to run in families.
- The rapid increase of myopia over the last 50 years seems to coincide with the increase in literacy and industrialisation in most countries.
- This could indicate that high near visual demands and visual stress may also be a causal factor in developing myopia in some individuals.
- The general conclusion is that myopia is due to a combination of genetic and environmental factors.
MYOPIA CONTROL
Myopia control is the area of science dedicated to slowing down or stopping the progression, or worsening of myopia in children and young adults. The following table is a compilation of over 30 research papers on myopia control, published up to and including 2013:
View This
MANAGEMENT ALTERNATIVES
Based on all the accepted research we recommend the following treatment options as most likely to stop or slow the progression of myopia:
GOOD VISUAL HYGIENE:
Good visual habits will reduce any near visual stress that may or may not be contributing to the development or progression of myopia. Either way, reducing near visual stress is a good thing for any visual system.
Good visual hygiene includes not getting too close to near work (not inside your knuckle to elbow distance)
Take regular breaks by looking away from your near work every 5 mins. If you notice a blur when you first look away it is time to take a longer break.
Avoid prolonged close work while tired or sick as this may also increase near point stress and stimulate more myopic development.
MORE OUTDOOR ACTIVITY:
A child with two myopic parents is at a six times greater risk of becoming myopic than a child with no myopic parents. A child with one myopic parent is at three times greater risk. This can be true even if you (the parent) didn’t become myopic as a child. Myopia can also occur without any family history at all.
A recent Australian study found that students who combined high levels of near work with low levels of outdoor activity were more likely to become myopic, whereas students who combined low levels of near work with high levels of outdoor activity were more likely to stay long sighted.
This was confirmed by a Singapore study which also found that lower amounts of outdoor activity increased the odds of becoming myopic.
SPECTACLE LENSES OR CONTACT LENSES TO REDUCE PERIPHERAL HYPEROPIC BLUR:
In a myopic person, the central retina is myopic, but the peripheral retina is actually hyperopic, or long sighted. It is thought that this stimulates the eyeball to grow causing the myopia to increase.
Some new spectacle and contact lens designs aim to reverse detrimental peripheral optics so that the peripheral focus is on, or in front of, the retina – similar to a non-myopic child.
SPECTACLE LENSES TO REDUCE NEAR VISUAL STRESS:
Wearing plus lenses (or less minus) for close work has the effect of reducing the focusing (accommodative) demand and makes it easier to keep the eyes turned in (converged).This will reduce near visual stress.
Studies have found this can be an effective way of slowing / reducing the rate of myopic progression.
ORTHO-K:
The OrthoK technique uses special hard contact lenses which change the curvature of the cornea to neutralise the myopic prescription.
These lenses are worn all night and removed each morning.
Latest clinical and scientific research shows that OrthoK can slow the progression (worsening) of short-sightedness, or myopia, in childhood by around 50%. In some children OrthoK can even halt the progression of myopia.
ATROPINE TREATMENT:
Atropine is an eye drop used to dilate the pupil and temporarily relax the eyes’ focusing mechanism. It has long been acknowledged that atropine also reduces the progression of myopia.
Recently it has been shown that low-concentration atropine gives the benefit of slowing the myopic progression without the visual side-effects.
Based on all the accepted research we recommend the following treatment options as most likely to stop or slow the progression of myopia:
An eye with no astigmatism is perfectly spherical in shape, like a marble. An astigmatic eye has a distorted shape, slightly like a football or grape. This can cause the image formed at the back of the eye to be distorted. Most people have a low degree of this condition originating in either the cornea or the lens inside the eye. Low degrees can slightly distort your vision, for example a ‘C’ may look like an ‘O’ or a ‘G’. You may also experience strain or discomfort with visual concentration. In higher degrees, astigmatism can cause images at all distances to be distorted or blurred.
Thankfully, it is easily corrected with spectacles or contact lenses.
Usually, astigmatism stays relatively stable throughout life, however there are some conditions that continue to progress. The most common one is keratoconus.
Keratoconus is caused by a thinning of the front surface of the eye, the cornea. This thinning causes the cornea to rapidly change shape creating high degrees of astigmatism and distortion. People with keratoconus may need hard contact lenses to obtain clear vision, or may need a surgical procedure to stabilise their cornea. Research has shown that eye rubbing (usually due to allergies like hay fever) can progress this condition.
WHAT IS PRESBYOPIA?
This condition usually occurs around the age of 40, and you’ll notice that your arms just don’t seem to be long enough anymore.
A normal aging process, called presbyopia, occurs around age 40. It is believed to stem from a gradual thickening and loss of flexibility of the natural lens inside your eye. These age-related changes occur within the proteins in the lens, making the lens harder and less elastic over time. Age-related changes also take place in the muscle fibers surrounding the lens. With less elasticity, the eye has a harder time focusing up close.
THE FACTS
1. You can’t escape presbyopia, even if you’ve never had a vision problem before reading glasses.
2. Eye exercises will not stop or improve the lens flexibility as it is a change in the lens protein.
3. Wearing reading glasses will not stop or accelerate this process.
4. As you get older your readers will need to get stronger.
5. Even people who are nearsighted will notice that their near vision blurs when they wear their usual eyeglasses or contact lenses to correct distance vision.
SYMPTOMS AND SIGNS
As people develop presbyopia, they find they need to hold books, smartphones and other reading materials further away. Eventually you may need to hold material at arm’s length in order to focus properly. When they perform near work, such as embroidery or handwriting, they may develop headaches, eye strain or feel fatigued.
WHAT IS HYPEROPIA?
Hyperopia, or Long-sightedness, causes a person to see clearer at far than at near.
The more hyperopic you are the greater the effort required by the focusing system to keep your close work clear. This can result in eye strain and fatigue. This “strain” can manifest itself as headaches after close work, blurred near vision, tired eyes, difficulty adjusting focus from distance to near then near to distance, avoiding close work and short attention span for near tasks. This can be especially true for children starting school with a significant degree of long-sightedness.
SYMPTOMS
Common symptoms are associated with tasks which require continued visual concentration. It becomes a problem to maintain a clear focus on near objects; causing headaches and tired or aching eyes.
In some age groups a prescription for hyperopia often works to relieve the strain, rather than clearing the vision. This is sometimes calle Accommodative Dysfunction. These ‘stress relieving lenses’ may only be required for a short period in a child’s life as they develop better accommodative stamina.
WHAT IS DRY EYE?
Dry eye is a condition where a person doesn’t have enough quality tears to lubricate and nourish the eye.
Dry Eye is when the tears that coat the surface of the eye are inadequate. Dry Eye does not necessarily mean that the eye is dry. In fact, you can still have dry eye with tears streaming down your cheeks! Dry eye just means the quality of the tear film is poor. This can mean the tears are too watery – which causes them to run down your cheeks – or alternatively, tear production may be reduced.
The tear film plays a vital role in providing nutrients to the front of the eye, in clearing the eye of dust and pollutants and providing clear vision. Without treatment, dry eye can lead to chronic irritation, inflammation, recurrent infections, and impaired vision.
SYMPTOMS AND SIGNS
Common symptoms of dry eye include:
- Irritation – Gritty, Sandy, Burning, Stinging, Itchy
- Inflammation – Red Eyes
- Watery Eyes
- Eye Fatigue – Heavy Eyes, Wanting to Close Eyes for Relief
- Light Sensitivity
- Blurry Vision
- Sticky Eyes, Particularly of a Morning
- Crustiness Around the Base of the Eyelashes
CAUSES
Some of the common causes for dry eye include:
- Smoking
- Age
- Contact Lenses
- Environmental – such as air conditioning, computer screens, dusty environments or low humidity
- Medical Conditions – such as arthritis, autoimmune diseases, sjogren’s syndrome and rosacea
- Hormonal Changes – often the cause of dry eye in postmenopausal women.
- Eye Problems – such as blepharitis (inflammation of the eyelid margins) floppy lids, and poor blinking habits
- Medications – such as antihistamines, birth control pills, antidepressants, blood pressure medication
Interestingly, dry eye has become much more prevalent in the last decade. Is this due to dietary changes? Or is it a result of the extra time we spend these days in front of screen based technology? The exact reason is still unknown; however, what we do know is that dry eye has become extremely common in today’s society, and it reduces the quality of life for those who are unlucky enough to have it.
TREATMENT
Dry eye can range from occasional mild irritation, to constant debilitating discomfort. The mild forms of dry eye can often be relieved with the occasional use of artificial tears. The more severe, chronic forms of dry eye will usually need more than just drops. In fact, often using more and more drops can make things worse as they will wash away the essential nutrients that your natural tear film provides. Treatment may include:
- Targeted Ocular Lubricants
- Dietary changes and supplements, including Omega-3’s
- Natural antibiotics and anti-inflammatories, such as Manuka Honey
- Prescription Medication (drops and tablets)
- Lid Hygiene, including treatment for demodex
- Lid Procedures including; treatment and expression of the oil producing glands in the lid (for Meibomian Gland Dysfunction) and BlephEx for treatment of blepharitis.
- Tear Duct Plugs
Dry eye can be a chronic condition for which there is no absolute cure. However, a comprehensive dry eye assessment and targeted treatment can successfully manage the condition so that your eyes remain clear and comfortable each day.
Hansen Optometrists run a comprehensive
dry eye clinic
with Justin Clunas.
WHAT IS DIABETES?
Diabetes is a chronic disease that occurs when there is too much glucose in the blood. This happens because the body is not producing insulin or not using insulin properly.
This condition comes in two types:
Type 1
– this represents 10-15% of all cases
Type 2
– is more likely in people with a family history
THE FACTS
- 280 Aussies develop this condition every day which equates to 1 every 5 minutes.
- 1.7 million Aussies are living with this condition right now.
- Diabetes is the leading cause of premature blindness.
TYPE 1
Type 1 occurs when the pancreas no longer produces insulin. This is one of the most common chronic childhood diseases in developed nations and requires insulin therapy. This form of diabetes is not caused by lifestyle factors however it is on the rise by 3% a year.
Diagnosis usually comes in childhood or as a young adult, although it can occur at any age.
Symptoms usually have an abrupt onset. They can include excessive thirst and urination, unexplained weight loss, weakness, fatigue and irritability.
TYPE 2
Type 2 occurs when the pancreas is not producing enough insulin or the insulin is not working effectively. Risk factors in developing type 2 include; family history, being overweight (from unhealthy eating and lack of physical exercise). Type 2 diabetes represents 85-95% of all cases, it is managed with lifestyle adjustments, this may require insulin therapy and diabetes medication.
Diagnosis usually comes in adults over the age of 45 but is increasingly occurring at a younger age.
Symptoms sometimes go unnoticed as the disease develops gradually. symptoms may include any of those for type 1 diabetes plus blurred vision, skin infections, slow healing, tingling and numbness in the feet.
WHAT DOES THIS CONDITION DO TO MY EYES?
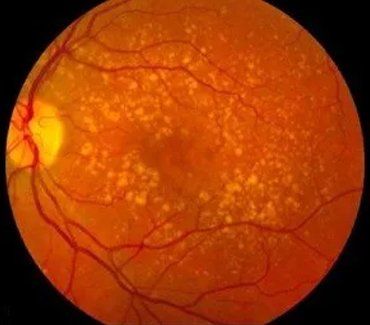
Diabetes can cause leaky blood vessels in the eye. 29% of Australians living with this condition have some form of Diabetic Retinopathy with 4.2% of those having Proliferative Diabetic Retinopathy.
- Non-proliferative Diabetic Retinopathy (NPDR) – this includes micro aneurysms, haemorrhages, hard exudates, cotton wool spots, and other vascular signs like bleeding.
- Proliferative Diabetic Retinopathy (PDR) – this includes pre-retinal or vitreous haemorrhages/new blood vessels, bleeding near the macular and clinically significant macular oedema.
For this reason it is really important to monitor patients and see them every 12 months (or less if required).
WHAT IS MACULAR DEGENERATION?
Macular Degeneration (MD) is a progressive eye disease in which the photoreceptors at the macular start to deteriorate and die due to the breakdown of the retinal pigment epithelium (RPE). This causes a build-up of retinal metabolic waste that clinically appears as yellow spots, called drusen.
The retina is the layer at the back of the eye which has light-sensitive pigment cells called photoreceptors. The macula is a small area of the retina where you focus an image of what you are looking at. It has the highest concentration of photoreceptors which provide us with our best eyesight ability and give us our colour perception. Underneath the macular is special layer called the retinal pigment epithelium (RPE). This layer provides nutrients and oxygen to the photoreceptor cells and removes the retinal metabolic waste products. As the photoreceptor cells are firing all the time while your eyes are open, they require lots of nutrients and produce lots of waste products.
WHAT DOES THIS CONDITION DO TO MY EYES?
MD results in the loss of central vision and has the potential to severely impact our daily lives by affecting our ability to read, drive, recognise faces and discriminate fine detail. There are two main forms of macular degeneration: commonly known as ‘dry’ and ‘wet’.
DRY MD
Characterised by a slow, progressive loss of the RPE cells due to the build up of drusen at the macula. This makes up about 85% of moderate to advancedMD cases resulting in a gradual deterioration of the central vision. Diet and a special formulation of vitamins and high-dose antioxidants, such as MD eyes have been shown to slow down the progression of MD in those with moderate to advancedMD in at least one eye.
View This
WET MD
This affects about two-thirds of advanced MD patients. This occurs when abnormal blood vessels grow underneath the macular and these vessels can spontaneously bleed, leading to a sudden loss of vision requiring immediate medical treatment. Treatment often requires regular injections to shrink the blood vessels.
View This
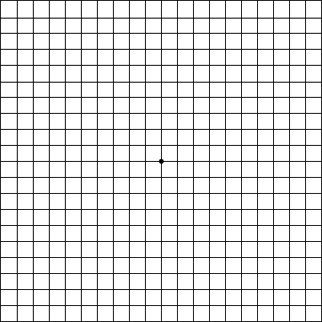
AMSLER GRID
It is important to note that dry MD can convert to the wet form of MD, which then requires prompt treatment. It is essential for all MD patients to monitor their macular quite closely with an Amsler Grid (seen on right), and to see their eye health professional regularly.
In Australia, approximately one in seven over the age of 50 have some element of MD which then contributes to 50% of all legal blindness.
We are seeing this more frequently because we are living longer, not always eating the right foods and not exercising regularly.
WHAT CAUSES MACULAR DEGENERATION?
- Age
- Family history of MD
- Smoking
WAYS TO PROMOTE MACULAR HEALTH:
1.
After 50 yrs of age old have your eyes and macular checked regularly every two years by your optometrist.
2.
Abstain from smoking.
3.
Have a well-balanced diet: include fresh fruit and vegetables (especially green leafy vegetables) daily, oily fish 2 to 3 times a week handful of nuts a week, and limit fat intake and high-GI carbohydrates.
4.
Exercise regularly and maintain a healthy body weight.
5.
Have adequate sun protection for your eyes.
For more information on Macular Degeneration visit the
Australian Macular Disease Foundation website.
WHAT IS GLAUCOMA?
Glaucoma is the name given to a group of eye diseases in which the optic nerve at the back of the eye is slowly destroyed. This results in loss of peripheral vision. If left untreated, it leads to tunnel vision and eventual blindness. The most common type of glaucoma is due to an increase in the pressure inside the eye (primary open angle glaucoma). This is usually due to either blockage of the circulation of fluid inside the eye, or a problem with its drainage.
SYMPTOMS
Glaucoma usually has no symptoms at all, and if we do notice it is often too late. There is often no pain experienced, and central vision is unaffected until the late stages of the disease. This is why this disease is often called the “invisible disease”. Sadly, people with glaucoma can remain unaware of the problem until it is too late – a large portion of their vision has already been destroyed and this damage is irreversible. For this reason, it is crucial to have regular eye health checks to ensure early detection of the disease.
New technology such as Optical Coherence Tomography (OCT) can detect optic nerve damage far earlier than previous methods. If you are in a high risk group, regular OCT will ensure detection of the disease before there has been any loss of peripheral vision. For most people, it is recommended to have an eye check for glaucoma by the age of 40 with ongoing two yearly regular eye health checks.
Anyone can get this disease, however there are people with increased risk of developing this disease, such as those with;
2. Diabetes
3. Migraine sufferers
4. High short-sightedness (myopia)
5. High long-sightedness (hyperopia)
6. Some eye injuries
7. High blood pressure
8. Use of cortisone drugs (steroids)
9. African & Asian descent.
TREATMENT
Treatment is aimed at reducing the pressure inside the eye. This can include regular eye drops, laser and even surgery. Treatment cannot recover what has been lost, but it can arrest, or at least slow down the damage process. That is why it is vital to detect the problem as early as possible, so that treatment can commence before too much vision is lost. For further information visit Glaucoma Australia at
www.glaucoma.org.au
LOWER YOUR RISK
Live a healthy lifestyle – that includes regular exercise and nutrition filled diet. There is no scientific evidence suggesting that certain vitamins and minerals prevent glaucoma or delay its progress. However, carotenoids (especially lutein and zeaxanthin), antioxidants (vitamins C and E), vitamins A and D, zinc and omega-3 fatty acids may all contribute to better vision.
Eat the alphabet:
- Vitamin A – found in carrots, sweet potato, mangoes, milk and egg yolks.
- Carotenoids – found in dark green, yellow and orange fruits and vegetables, including spinach, broccoli, green beans, papaya, oranges, mango, sweet potato, corn, peaches and apricots.
- Vitamin C – found in citrus fruits, tomatoes, strawberries, leafy greens, sweet and white potato, broccoli and capsicum.
- Vitamin D – found in cod liver oil, ‘oily’ fish, fortified milk, cereal and egg yolks.
- Omega-3 fatty acids – found in salmon, sardines, walnuts and flaxseed oil.
- Zinc – found in oysters, red meat, poultry, beans, nuts, whole grains and dairy products.
WHAT IS CATARACTS?
A cataract is a clouding of the clear lens in the eye and is one of the leading causes of vision impairment in Australia and the world.
We all will develop this condition to some degree if we live long enough. It is part of the normal aging process of the lens inside our eye.
As the lens ages it becomes less flexible (why most people will need reading glasses around 40 years of age) and slowly goes cloudy. Cataracts affect both eyes, but usually asymmetrically. As this condition develops, colours can become washed out, vision deteriorates, halos can form around lights (especially at night), there can be an increase in glare, and cause poor vision at night.
This condition can occur at birth, but can also be due to trauma, radiation exposure, or as a result of eye surgery. It can develop earlier in diabetics, smokers and in people who have had prolonged exposure to sunlight.
PREVENTION
Ways to prevent or slow the development of cataracts include wearing sunglasses to reduce your UV light exposure, and not smoking. The blur associated with early cataracts can often be improved with spectacles. Surgery is considered once your vision, with the best glasses possible, is impacting your day-to-day life. Surgery removes the cloudy lens and replaces it with an artificial lens and is the only long term effective treatment.
If you are not sure if you have cataracts make an appointment for an eye health assessment.
For more information about cataracts, visit the Vision Australia link here.
WHAT IS OCULAR THERAPEUTICS?
A therapeutic optometrist is approved to provide treatments where appropriate to their patients. Sometimes a therapeutic optometrist will also work in conjunction with an Ophthalmologist (a specialist in medical and surgical eye problems) to treat a patient, particularly in the case of glaucoma.
WHO REQUIRES THIS TREATMENT?
For people with eye infections, major eye allergies, eye disease and glaucoma, therapeutics (medicines for the eye) are often required.
PHARMACEUTICAL BENEFITS SCHEME (PBS) & OCULAR THERAPEUTICS
Pharmaceutical Benefits Scheme subsidies generally apply for ocular therapeutic products prescribed by therapeutic optometrists.
To obtain this endorsement, optometrists are required to complete mandatory training and apply for registration to prescribe therapeutics from their state board.
The optometrists at Hansens Eyecare Plus work hard to keep up to date with the latest technology, training and qualifications. Justin Clunas, one of our full-time optometrists has completed his Graduate Certificate in Ocular Therapeutics and is able to prescribe ocular medications where necessary.
WHAT IS NUTRITION?
Nutrition is the process of providing or obtaining the food necessary for health and growth. It plays a major role in overall health of the body and heavily impacts our vision.
Poor diets with highly processed foods and large amounts of salt or sugar can increase the risks of developing a number of eye diseases and other health problems that could lead to blindness. For healthy vision through life you need to make sure diet consists of plenty of vitamins, fresh fruits and vegetables.
5 FOODS FOR HEALTHY EYES
ALMONDS
A rich source of vitamin E, zinc, fibre, iron, magnesium and potassium, almonds are amazing for overall health and well-being in the whole body. Research has shown this super nut can actually slow down the progression of macular degeneration.
CITRUS FRUIT AND BERRIES
The ultimate sources of vitamin c, citrus and berries, especially blueberries, are considered the healthiest food for your eyes. These also contain high quantities of vitamin A, C, E, and zinc, which have been shown to reduce risk of developing cataracts and macular degeneration.
LEAFY GREENS
Leafy greens such as; cooked spinach and kale, broccoli, collards and turnip greens contain high amounts of lutein and zeaxanthin. These antioxidants have shown to lower risk of development of macular degeneration and cataracts, whilst also reducing glare discomfort, enhancing contrast and increasing visual range.
FATTY FISH
Fatty fish such as; tuna, salmon, mackerel, anchovies and trout are rich in DHA, which is an acid found in the retina. Fatty acids may also help protect eyes from macular degeneration and dry eye. These essential fatty acids help drain fluid from the eye thus decreasing the risk of high pressure and glaucoma.
EGGS
Eggs, as we all know are packed full of protein, but did you know that they are also provide us with lutein, vitamin E and omega 3. Egg yolks also contain zeaxanthin which is believed to help protect eyes against UV radiation from the sun.
These benefits help reduce the risk of developing cataracts and fight macular degeneration.
LOWER YOUR RISK
We love good healthy food here at Hansen Optometrists, and that’s why we have put together a bunch of great little recipes to keep your eyes healthy all year round! Simply click the link.
Eye Healthy Infused Water
Chicken and Almond Wrap
Sweet Potato and Peanut Soup
Classic Pumpkin Soup
Roasted Parmesan and Balsamic Cauliflower
Minestrone Soup